AGEP vs GPP: When Skin Reactions Look Similar but Behave Very Differently
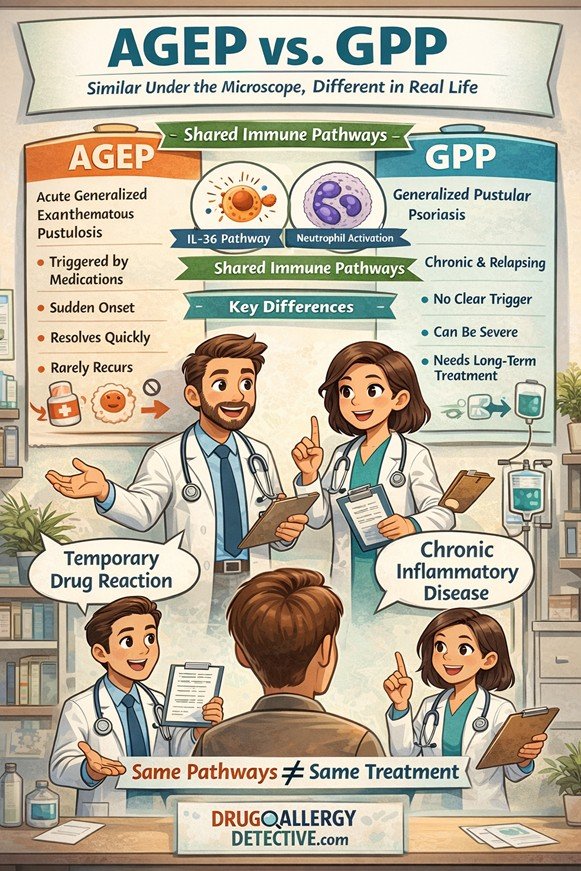
Skin rashes can be alarming, especially when they appear suddenly and spread quickly. Two conditions that often cause confusion are acute generalized exanthematous pustulosis (AGEP) and generalized pustular psoriasis (GPP). AGEP vs GPP is a comparison that often raises confusion among both patients and clinicians. These two skin conditions can appear strikingly similar at first glance, yet their causes, clinical behavior, and long-term management are very different.
Understanding these differences is important — not only for accurate diagnosis, but also for choosing the right level of treatment and avoiding unnecessary risk.
They may look similar on the skin.
They may even look similar under the microscope.
But in real life, they behave very differently.
What are AGEP and GPP?
AGEP (Acute Generalized Exanthematous Pustulosis)
AGEP is a severe cutaneous adverse reaction (SCAR), most often triggered by medications such as antibiotics or other commonly used drugs.
It typically appears suddenly, with widespread small pustules on red skin, often accompanied by fever or discomfort. Although it is classified as a severe drug reaction, the good news is that its mortality rate is low, and most patients recover quickly once the offending drug is stopped.
Because of this, AGEP is considered serious but usually self-limited when recognized early.
GPP (Generalized Pustular Psoriasis)
GPP is a chronic inflammatory skin disease that may occur with or without a clear trigger. Unlike AGEP, it often follows a relapsing course and can become life-threatening if not treated properly.
Patients with GPP may require long-term treatment, including biologic therapies, to control inflammation and prevent complications.
Why are AGEP and GPP being discussed together?
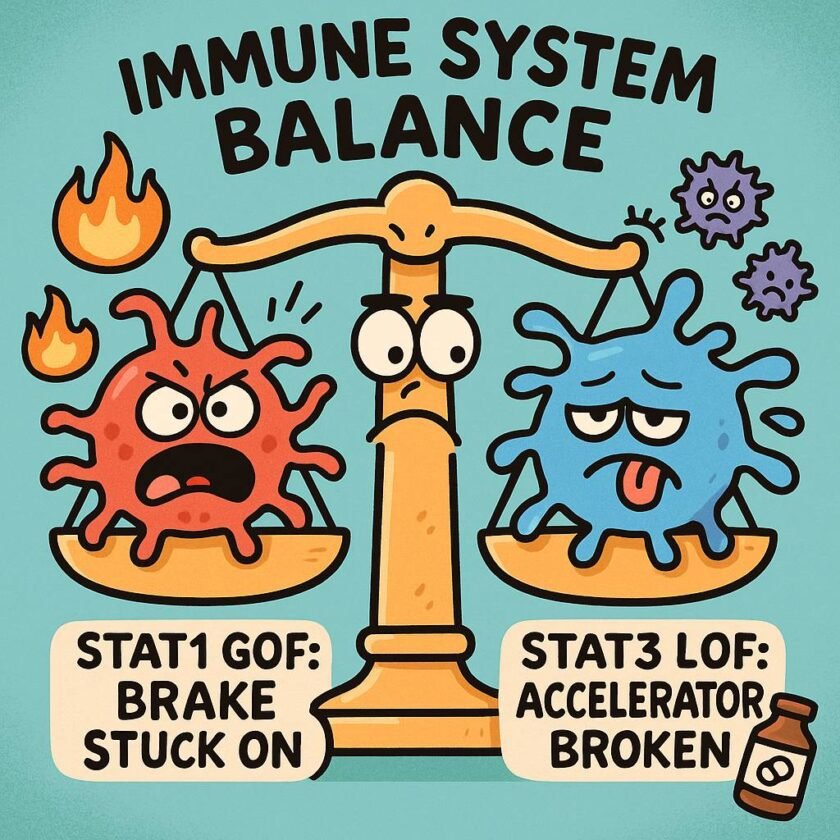
A recent study published in The Journal of Allergy and Clinical Immunology found that both AGEP and GPP activate similar immune pathways — particularly the IL-36 inflammatory pathway.
Because of this overlap, the authors proposed that AGEP might represent a drug-triggered form of GPP.
From a biological standpoint, this idea makes sense.
From a clinical standpoint, however, the picture is more complex.
Why real-life behavior still matters
Even when two diseases share immune mechanisms, their clinical behavior can be very different.
AGEP typically:
- Occurs shortly after starting a new medication
- Is considered a severe drug reaction, but usually resolves quickly
- Rarely recurs unless the same drug is reintroduced
GPP, in contrast:
- Often develops without an obvious trigger
- Tends to relapse over time
- Can be severe or life-threatening
- Often requires long-term systemic or biologic therapy
These differences are critical when deciding how aggressively to treat a patient.
AGEP vs GPP: Key Clinical Differences
| Feature | AGEP (Acute Generalized Exanthematous Pustulosis) | GPP (Generalized Pustular Psoriasis) |
|---|---|---|
| Primary cause | Usually drug-induced (e.g., antibiotics, antifungals, others) | Often idiopathic or genetically predisposed |
| Onset | Sudden, usually within days after drug exposure | May be sudden or gradual, often without a clear trigger |
| Disease course | Acute and self-limited | Chronic or relapsing |
| Recurrence | Rare (unless the same drug is reintroduced) | Common |
| Severity | Considered a severe cutaneous adverse reaction (SCAR), but usually self-limited | Can be severe or life-threatening |
| Systemic involvement | Usually mild and transient | Can be severe (fever, systemic inflammation, organ involvement) |
| Typical treatment | Drug withdrawal, supportive care | Systemic therapy often required |
| Role of biologics | Rarely needed; reserved for severe or refractory cases | Often essential for disease control |
| Immune mechanism | Drug-triggered immune activation | Chronic autoinflammatory process |
| Long-term management | Usually not required | Often required |
| Overall prognosis | Excellent once the drug is stopped | Variable; may require lifelong management |
Why this distinction is important
Although AGEP belongs to the group of severe cutaneous adverse reactions, it is usually self-limiting once the causative drug is withdrawn.
GPP behaves very differently. It is a chronic inflammatory disease that often requires ongoing treatment and close monitoring.
Treating AGEP the same way as GPP could expose patients to unnecessary medications and risks — even though the skin findings may initially look similar.
AGEP and GPP may share immune pathways, but their clinical behavior, severity, and treatment needs are very different.

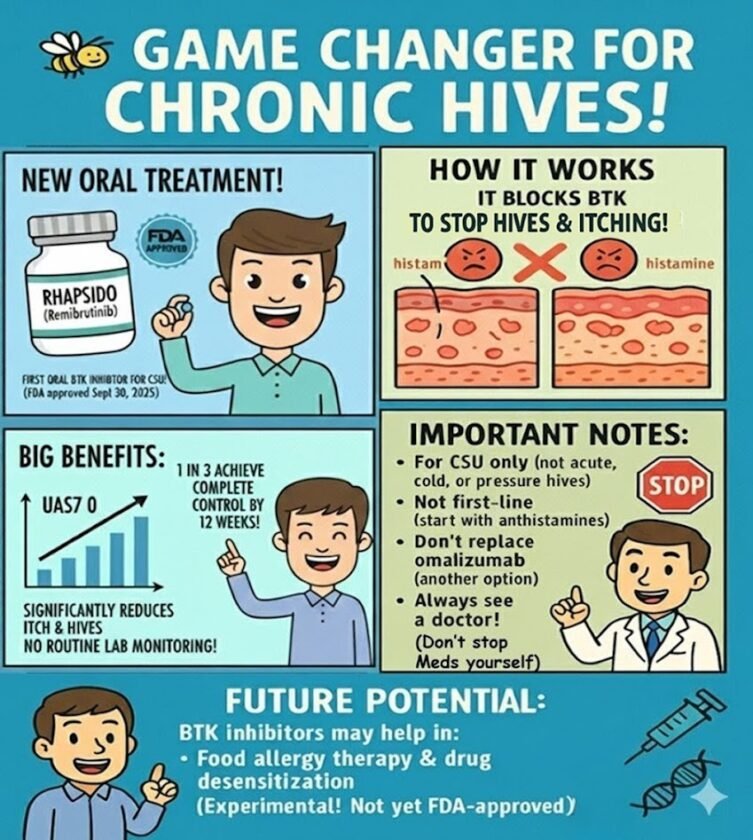
What about newer treatments like IL-36 blockers?
IL-36–targeted therapies, such as spesolimab, have transformed the management of GPP and can be life-saving in severe cases.
In rare situations, these treatments may be considered for very severe or refractory AGEP. However, for most patients, supportive care and drug withdrawal remain sufficient.
The key principle is balance:
treatment should reflect disease behavior, not just molecular similarity.
A practical way to think about it
Rather than viewing AGEP and GPP as the same condition, it is more helpful to see them as part of a shared inflammatory spectrum.
- Some patients experience a short-lived drug reaction.
- Others have an underlying inflammatory tendency that leads to recurrent disease.
Recognizing where a patient falls on this spectrum allows for safer and more personalized care.
The takeaway
- AGEP is a severe drug reaction, but usually short-lived and reversible.
- GPP is a chronic inflammatory disease that often requires long-term treatment.
- They may look similar, but they behave very differently.
- Good medical care means matching treatment to disease behavior, not just appearance.
Quick summary (for busy readers)
- 🧬 AGEP and GPP share immune pathways
- ⚠️ AGEP is a severe drug reaction, but usually resolves quickly
- 🔁 GPP is chronic and often relapsing
- 💊 Treatment should reflect disease behavior, not just biology
References
- Benezeder T, Bordag N, Woltsche J, Falkensteiner K, Graier T, Schadelbauer E, et al.
IL-36–driven pustulosis: transcriptomic signatures match between generalized pustular psoriasis (GPP) and acute generalized exanthematous pustulosis (AGEP).
J Allergy Clin Immunol. 2025;155:1913–1927. - Choon SE, Bachelez H, Wang CW, Chung WH.
AGEP and GPP share immune mechanisms but have different clinical courses.
J Allergy Clin Immunol. 2025.